Recently, Setra hosted a webinar around protecting isolation rooms during the coronavirus pandemic. The speaker was a member of our sales team who is Setra's Critical Environments specialist. Below are answers to the questions asked throughout the webinar.
Creating Temporary Isolation Rooms
If I don't have enough isolation rooms in my hospital, what are my options?
Many hospitals and facility mangers are familiar with the HVAC design of their hospital. If they're familiar with that design, they know what parts of the hospital they can adequately pressurize, but in floors where you don't have a particular pressure plan, the pressure zones might be neutral between rooms and hallways. Driving additional pressure into the common areas through the HVAC system can increase the airflow to those common areas. This pushes additional air into the patient rooms and creates negative pressure zones. The room would then need to be measured with a room pressure monitor or a handheld manometer. There are techniques to ensure a room is negatively pressurized without devices as well. With the door closed, you can tear off a piece of tissue, drop it by the bottom of the door, and if its pulled into the room, the room has a negative pressure. Those are some techniques that can be used to try to pull some rooms negative that aren't designed as isolation rooms.
Are there parameters beyond negative pressure that should be monitored in isolation rooms?
The most important one is the differential pressure between the room and the hallway or the adjacent space. This guarantees the isolation room is negative. The next most important condition is the air change rate. By ASHRAE 170 code, that air change rate should be around 15 air changes per hour (ACH). That's a design guideline more for HVAC design rather than patient safety, but the air changes should be verified through facility management that its sufficient. Temperature and humidity are really just for the comfort of the patient. The bottom line is differential pressure is the most important condition for isolation rooms.
I have to use temporary construction spaces because I don't have enough beds in my hospital. How do I make those rooms safe?
Temporary spaces, especially in parking lots or even wards inside a hospital, aren't designed to be negative pressure zones. I would say, just to recap, if its inside the hospital you might be able to drive additional air into patient rooms; then, measure that air with a device that gives a visual pressure reading. If its an outdoor space, probably the most common thing to do is to use an exhaust fan that is inside the room, pushing air outdoors. That way even with tented areas and temporary construction, you'd be able to pull a room negative. The air that's exhausted outdoors is potentially hazardous, so you want to cordon off an area and make sure there is sufficient exhaust dispersion into the air so no one passing by that exhaust fan could potentially be contaminated. You'd have to be pretty close to do that, but an abundance of caution is the advice today.
Could you expand on potential temporary solutions for isolation rooms given the current conditions with COVID-19?
Any of Setra's monitors can be mounted in a temporary enclosure and hung on a wall, whether that wall is a permanent wall in the facility or a temporary wall. The wall only needs enough structure to support the bit of weight from the device. Just bring 24V of power to that device, and that can be run in simple temporary raceways that are put up; these are plastic raceways you can run wires in. Then bring your differential pressure tubing to one side or the other. All the devices, all the room pressure monitors, that Setra sells today include everything in the kit for a full solution of differential pressure monitoring, especially if there is audible alarming needed. Even in temporary situations with flexible walls there would need to be some sort of structure to support the device, but a speed box for a single gang can support the Lite and the SRPM.
Proper Isolation Room Ventilation and Airflow
Would you suggest using a smoke tube to visualize how air is being distributed with each room for the caregiver and patient's protection?
If they have a smoke generation device, that should be used daily in the facility, especially in areas where there isn't a room pressure monitor giving a value of what the differential pressure setting is. But like I mentioned earlier, facilities that don't have that kind of device can use a simple tissue, drop it down, and if it gets pulled in, that's effectively the same thing as using a smoke trail. In other facilities, a common device used is a handheld manometer. With a handheld manometer, put the tube down by the door cut into the room and do a visual verification on the meter itself. There are several ways that with low tech and higher tech devices to verify that those rooms are negative pressure.
Some customers have tried limiting supply air to increase the negative pressure. Shouldn't they be trying to increase exhaust first?
It's really about the overall balance of the room and the air change rate. The proper way to do this is really with a rest and balance company to verify that you're not stealing too much air from adjacent areas. However, either technique, increasing exhaust or limiting supply, as long as your goal is to maintain that 15 ACH, either one of those techniques will do.
Can additional air changes reduce in room contamination generated by infectious patients that are not intubated?
There have been various studies about increasing the air change rate and its efficacy on handling airborne pathogens. In general, increasing the number of air changes is a good thing, but the guideline for the minimum for the isolation rooms is 15 ACH. You can increase that to 20 or 25 perhaps, but beyond that the number of air changes could potentially steal air from other rooms and upset the overall balance of airflow. In some cases, it could pull negative rooms positive to compensate for the additional air required in other areas. I would caution against using a blanket approach to increasing air changes. Stick to the guidelines of 15 to 20 ACH for these rooms because those guidelines in ASHRAE 170 are based on quite a bit of research.
Is natural ventilation worth considering for air ventilation if the pathways are controlled?
Generally no, but in emergency situations perhaps yes. In layman's terms, natural ventilation is having either additional fresh air coming in through the supply air or having a window open. If a window is open then it has to be open just a slight amount in order for the room to be under negative pressure, and you would need to drive some sort of fan in order to exhaust the air out that window. You want to also make sure that window is taped off so no air is coming in through wind or drafts as well as ensure that window is not near a sidewalk or other areas where you could potentially infect people who might be walking by.
Setra's Products Can Help
What does Setra have for temporary installs or portable units to verify temporary rooms are negative?
Most of the solutions we have today are designed for permanent mounting. The Setra Lite and Setra SRPM are surface mount units that can be put into a single gang box and need only 24V power to function.
Since hosting this webinar, Setra has released two new Setra Lite Kits to help with preparing temporary isolation rooms. The Quick Mount Kit includes a Setra Lite, a mounting bracket, RPS single gang filtered pressure port, AC power adapter with a 6-foot cord, and four 9V batteries. The Quick Mount Kit can be powered with either the AC adapter or the battery pack. The Portable Kit includes a Setra Lite, 10-feet of filtered medical grade tubing, and battery pack with four 9V batteries. For more information on these kits, click here.
What Setra products would you recommend for permanent install in new isolation rooms?
For new isolation rooms that are being designed there is an ASHRAE 170 guideline that says that device must have both visual and audible indication of alarm conditions. The flagship product for Setra is the Setra FLEX, which is a 7" touchscreen room pressure monitor. It can verify those 2 conditions that I said were fairly important for isolation rooms, the differential pressure and the air change rate, and also show observations of temperature and humidity for the comfort of the patient. The SRCM and SRPM also both have visual and audible indications, and those products are suitable and code compliant for monitoring isolation rooms.
Some nurses/doctors get annoyed by the alarm that gets generated when a door in an isolation room is opened. Is there an accommodation/option for a time delay when the door opens?
All of Setra's products have this and if this particular customer has a non Setra product at their facility, they should look online to see if there is either a door delay or a method for accessing the touchscreen or any buttons on the device that might mute that alarm for a period of time.
What is the biggest differentiator of Setra Pressure monitoring systems to other pressure monitors available on the market?
I'd say the biggest differentiator is our capacitance based transducer, which is the sensor in the device. We've manufactured our sensors for over 50 years now, and we've refined this technology for the highest accuracy and the highest reliability. The sensor itself requires no flow through air, which with other devices can actually clog the sensing element with bed linen fragments. The Setra Sensor is a dead-ended sensor, so we're measuring the actual pressure in the room without having air flow through it. We do this with two sides of the sensor, one measuring the reference side and one measuring the room side. Then a digital value appears on the room pressure monitor. That's our main differentiator.
Additional Resources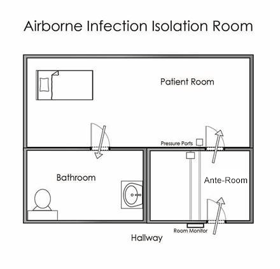
COVID-19 Room Monitoring Solutions Webinar
Keeping Hospitals Safe During Disease Outbreaks
Managing Accurate Pressurization in Isolation Rooms